How can I participate in physical activity to help manage my pain?
Start low and go slow
- If you have not been active in a while, consider starting at 10-25% of what you eventually want to do and slowly increase from there.
- For example, if you want to eventually walk for 40 minutes, try starting with a 4 to 10-minute walk. Once you have walked that amount several times, you can increase the amount of time of your walk by 10% or add about 1 minute to each walk over time.
- It might feel like you aren’t making progress, but you’ll be there before you know it! Starting slow can help prevent injury, soreness, and flares in your chronic pain symptoms.
- Starting low and going slow allows your nervous system, joints, and muscles to get used to the activity over time without having a pain flare.
- If you have been doing some physical activity here and there, but your pain flares up, consider using the 50% guideline to become more active.
- The 50% guideline means that you first identify how long you are active when your pain flares up. Then, cut that activity time or intensity down by 50%.
- For example, your eventual goal may be to do a 50-minute fitness class. But, right now, doing the class for 30 minutes causes your pain to flare for several hours or days. Cut down the 30 minutes bt 50% – try doing the class for 15 minutes to start.
- Then, increase the amount of time you participate by 10%, in this case by 2 minutes, after you can do the 50% without a flare. Keep increasing the time you participate steadily over time until you reach your goal.
- How much time you spend doing an activity is one way to change an activity. Learn about other options in the FITT principle section below.
- Building up the amount of activity you do over time will help you manage your pain, so that you can be active week in and week out!
Warm up and cool down
- Warming up and cooling down are essential to prevent injury and help you feel great when you’re physically active. Think of it like starting up your car in the winter. You need to let the engine get warm, so your drive is smooth. Your body works the same way!
- Consider a short warm up of stretching or walking to get your heart rate up. You also want to do a short cool down of stretching or gentle movement to help your body to recover.
Listen to your body
- You know your body best! A great way to prevent injury or over-doing an exercise is to listen to what your body needs. If you need food, water, sleep, or relaxation, your body will let you know, and it’s important to listen.
Use activity trials to find physical activities that you enjoy.
- Being active is about having fun! Try new activities to stay engaged and find what you like to do most. If the activity isn’t enjoyable, too easy, or too hard, then try changing it up with something new. Don’t feel you need to stick to one activity to see progress or to be active week in and week out.
Use the FITT principle to change your activity over time.
- The FITT principle is a great way to increase or decrease your level of activity. By changing the frequency, intensity, timing, or type of physical activity, you can create a plan that lets you meet your goals.
What is the FITT Principle? How do I use it?

Frequency refers to how often you are physically active. Most people living with chronic pain find that daily activity is the best way to manage their pain.
Intensity refers to how hard you work during the activity. If walking is your chosen activity, you can change the intensity by walking at a slower or faster pace, depending on how your body feels. If lifting weights is your activity, you can change lots of different things to make the intensity lower or higher, depending on how you feel. For example, you can reduce intensity by taking more time, lifting lighter weights, or doing fewer repetitions. Increase the intensity by taking less time in between exercises, lifting heavier weights, or doing more repetitions.
Time refers to the time you spend being physically active. If you’re doing a high intensity activity, reduce the time you spend on this activity when you’re not feeling your best. Lighter intensity activities can usually be done for a longer amount of time. Or if you feel good, then spend more time doing the higher intensity activity.
Type refers to what physical activity you choose to do. Try different activity options to find ones that you enjoy and challenge your body.

How do I know how intense each activity is?
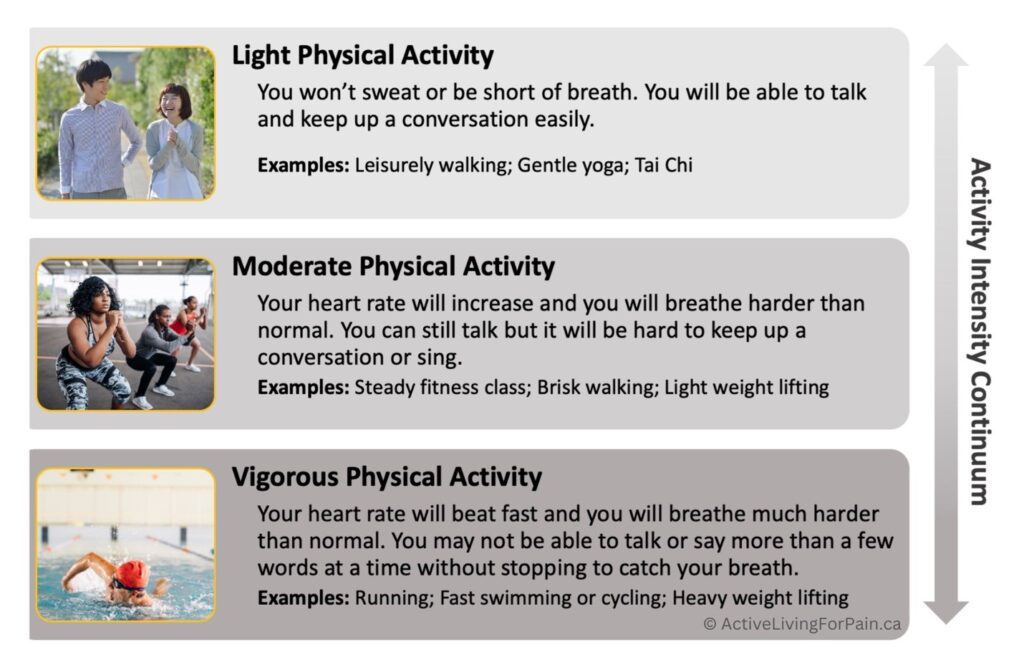
Physical activity can range from light to moderate to vigorous intensities. The best part is that all physical activity intensity levels can be incorporated in daily life! Light activities can help reduce pain and allow your body to recover from more intense activities so that you can be regularly active long-term. Moderate and vigorous activities produce several key health benefits including releasing natural endorphins that help you feel better, improve your pain, and enhance your quality of life. What activities are light, moderate, and vigorous can be different for different people based on their health and fitness levels, as well as their pain levels. You can use the descriptions along the activity intensity continuum below to determine how intense your physical activity is for you.
Leading a Physically Active Lifestyle – What Research
Shows Works
Being physically active week after week, month after month, year after year improves pain management. But being regularly active takes more than an initial commitment. Research shows that many people stop being active within 6 months of starting a physical activity routine.
Fortunately, researchers who study physical activity and pain have identified key skills that people can develop and use to be physically active for weeks, months, and years. These skills include:
- Self-monitoring of pain.
- Setting realistic physical activity goals.
- Overcoming physical activity barriers.
- Using the 4 P’s of pain self-management.
Self-monitoring of pain
Self-monitoring means keeping track of your pain symptoms before, during, and after being physically active. Self-monitoring can help some people determine when to be active and track your progress. Not everyone with chronic pain should track their pain symptoms. If you feel anxious when thinking about your pain levels, you may benefit from learning coping skills from a trained mental health care provider before doing this.
There are 3 key times to self-monitor your pain symptoms:
- Before you start your activity: Chronic pain levels can fluctuate throughout the day. Tracking your pain before being active can help you to know how your pain changes. Then, you can use this information to help you plan what time of the day you might be most likely to follow through and do your planned activity.
- While you’re doing your activity: Tracking your pain symptoms during different activities can help you learn which ones you enjoy doing and how your body reacts to the activity.
- After your activity is done: Tracking after your activity is done can help you to know which activities do or do not cause your pain symptoms to change or flare up. Over time, you can track how much activity you’re doing and whether your pain gets better or worse.
Goal setting
Goals are standards we set that guide our efforts as we work to accomplish them. We can make small goals throughout daily living to be more active. For example, parking a little bit further from the grocery store entrance. Goals can be larger and longer-term too. For example, how often do you want to be active 6 months from now? When it comes to physical activity, it is helpful to set SMART goals. SMART goals are specific, measurable, achievable, realistic, and timely.

Overcoming barriers
Barriers are factors that stop you from doing your physical activity. Barriers can occur in your daily life or be directly related to your chronic pain. Barriers can be challenging. However, you can think of creative ways to overcome them. The key to overcoming barriers is to first know what stops your from being active. Then, keep making different changes until you find solutions that work best for you!
Step 1: Identify the barrier(s) that make it difficult to be active.
Step 2: Try using a strategy to cope with the barrier to make being active possible.
Step 3: Monitor the strategy to identify if it is a solution to the barrier.
Step 4: If being active still isn’t possible, try using another strategy.
The key is to never give up – practice makes progress when dealing with barriers.
The 4 P’s of pain self-management
The 4 P’s include prevention, psychological, physical, and pharmacological strategies that can be used to help improve pain. The best results happen when you use a combination of different strategies.
Prevention strategies are ways you protect your body and nervous system to prevent your pain from worsening or leading to other health complications. These can include:
- Using mobility aides like a cane to improve balance, prevent falls, and reduce weight bearing on an inflamed joint
- Maintaining a healthy body weight to minimize the impact of daily activities on your joints
- Using a brace to support an unstable joint
Psychological strategies help manage pain through better understanding of mind-body connections including your pain-related thoughts, feelings, and behaviours. Our thoughts and feelings can affect our behaviour. Our behaviour can affect our thoughts and feelings. Because of this shared connection, we can change pain by changing how we think, feel, and respond to pain. Techniques that can be used include:
- Mindfulness-based activities
- Relaxation and stress management
- Breath control practices
Physical strategies involve using your own body to help reduce pain. They include active strategies, like movement to increase activity or reduce time being sedentary, or passive strategies where you work on your body, or a therapist treats your body to improve how it moves and works. Some passive physical strategies you can do to your own body include:
- Self-massage
- Applying warm or cold packs
Other physical strategies require a trained health care provider who can use hands-on therapies to help you affect your body tissues. Such hands-on therapies can include physiotherapy, massage therapy, chiropractic, osteopathy, or acupuncture.
Pharmaceutical strategies involve using medications that can either be prescribed by a doctor or be obtained over-the-counter at a local pharmacy. Different types of medications are used to treat different types of pain.
Opioids like codeine, morphine, oxycodone, fentanyl, and methadone are prescribed by a healthcare provider to manage pain. However, these are more useful for acute nociceptive pain (e.g., after surgery) and are not as helpful for chronic pain. Opioids can make some types of pain worse.
Over-the-counter medications can be helpful and include options like acetaminophen and nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen, aspirin).
Other medications prescribed for pain may include muscle relaxants, antidepressants, anti-epileptic medications, cannabis, or corticosteroids. Most medications are taken by mouth, but some medications are taken by injection or through patches, creams, or gels on the skin.
All medications have side effects and some medications, even ones bought over the counter can be harmful if you have another chronic health condition that affects your liver, kidneys, gastro-intestinal system, or heart.
Before starting a medication for your pain, check with your doctor, nurse practitioner, or pharmacist for advice on which medications are right for you.


